Industry News

Arlington, VA — Surescripts® released a new data report that highlights the biggest issues facing care providers, pharmacist prescribing trends and opportunities for patient care teams to continue evolving to meet the needs of patients.
“Barriers that limit health intelligence sharing between clinicians prevent the benefits of an evolving care team, like greater efficiency and more accessible care for patients, from being fully realized,” said Frank Harvey, Chief Executive Officer of Surescripts. “Policies are evolving at the state level to allow pharmacists to provide care at the top of their education and training. While this is a step in the right direction, a truly comprehensive policy shift is still needed to bring reimbursement and access to patient intelligence sharing in line with how care is being delivered today so that we can continue helping healthcare heal itself.”
Key Highlights:
- 85% of pharmacists and 76% of other clinicians (including physicians, physician assistants and nurse practitioners) ranked prescription medication costs as the top issue and 85% of pharmacists and 72% of other clinicians ranked burnout as the second biggest issue.
- Since 2023, a growing number of pharmacists (75%, up from 65% in 2023) and other clinicians (29%, up from 26% in 2023) agree with the statement: "we should allow pharmacists to take on more primary care duties like performing point-of-care testing and diagnostics, managing medications used to treat chronic conditions, and prescribing medications for certain conditions."
- About one-third of pharmacists feel their current position allows them to offer patients all the care they need (36%).
- Unlike other clinicians, more than 8 in 10 pharmacists regard connecting pharmacists and other clinicians with centralized clinical information about their patients as a high priority. (85% of pharmacists and 57% of other clinicians).
- Pharmacists and other clinicians agree that it is somewhat or very difficult to share patient information securely and confidently with other care providers (46% of pharmacists and 31% of other clinicians).
- The top 100 most active pharmacist e-prescribers were responsible for 561,054 new prescriptions nationwide in 2023. Pharmacists in California, New Mexico, and New York accounted for 52.9% of the total nationwide pharmacist-issued e-prescriptions.
Between 2022 and 2023, Surescripts’ analysis shows that e-prescriptions issued by a pharmacist have increased 13% and the number of pharmacists e-prescribing also increased 28.8% in the same timeframe.
“This new data shows that patients are driving demand for pharmacists to provide a broader range of clinical care services closer to home, but they need to be reimbursed for these services and gain access to key patient insights to ensure they can provide better quality, safe and less costly care,” said Shannon Reidt, PharmD, MPH, MS, BCPS, Director Medication Research and Analytics for Surescripts. “Given the primary care provider shortages we are seeing, it’s becoming more critical to advance policies that allow pharmacists to care for patients at the full scope of their education and training – which includes medication management for patients with chronic conditions and provide test-to-treat services for patients for routine illnesses.”

CHAPEL HILL, NC — RxLink™, a leading provider of medication affordability and price transparency solutions for healthcare systems, is excited to announce its strategic partnership with ConnectiveRx, a premier provider of patient support, affordability, awareness, and adherence solutions for branded and specialty prescription medications. This collaboration takes a patient-first approach, enabling healthcare providers to help patients reduce their out-of-pocket prescription costs by providing access to available savings options from pharmaceutical manufacturers and sending those directly to the patient via text. This allows patients to compare all available options—from pharmacy switches to insurance coverage and therapeutic alternatives—in real-time, often before leaving the provider's office, facilitating more informed, patient-driven discussions with their healthcare provider.
RxLink's innovative platform, MedMap™, delivers savings options directly to the patient in a user-friendly web interface at the point of care. Coupled with ConnectiveRx's robust portfolio of patient support programs, MedMap will help extend the care team's ability to easily identify the most appropriate and affordable options for patients and enable pharma brand teams to effectively drive awareness of affordability programs through hyper-targeted and personalized notifications based on diagnosis, payer strategy, demographics, etc. This is especially helpful for cost-sensitive patients who typically don't make it to the pharmacy counter despite having already been prescribed a particular therapy.
"By partnering with ConnectiveRx, RxLink reaffirms its commitment to improving patient outcomes and expanding access to affordable medications for all patients," said Joe Jackson, VP, Pharma Partnerships at RxLink. "ConnectiveRx's industry-leading portfolio of pharmaceutical manufacturer sponsored savings programs will further empower healthcare providers to support their patients without adding work to their plate. Our partnership objective is to ensure every patient can simply follow their doctor's orders by offering education and savings at a critical point in the care journey – while the patient is on the way to the pharmacy."
ConnectiveRx programs can equip both physicians and patients with real-time information on cost-saving opportunities for their prescribed medications.
"By integrating our platform with RxLink's extensive and fast-growing health system network, currently supporting over 20M patients, this partnership will enable physicians to play a proactive role in educating the patient, reducing medication costs, and improving overall patient satisfaction—all without adding any additional effort to the provider workflow," said Danielle Daly, Chief Marketing and Communications Officer, ConnectiveRx.
Together, RxLink and ConnectiveRx are committed to driving positive change in the healthcare industry by providing physicians with the resources and support they need to deliver high-quality, cost-effective care to their patients.
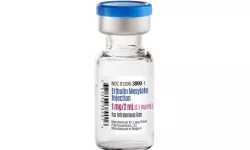
ROSEMONT, IL — Long Grove Pharmaceuticals, LLC, a supplier of differentiated pharmaceuticals, received Food and Drug Administration (FDA) approval for a generic Eribulin Mesylate Injection. Long Grove’s Eribulin Mesylate is an AP-rated chemotherapy medication bioequivalent to HALAVEN®.
“Our goal is to create more affordable pathways to pharmaceuticals. The introduction of a generic in a market where choices are limited is an important step to ensure patient access,” said Peter Karas, Chief Commercial Officer of Long Grove Pharmaceuticals. “We’re grateful for the opportunity to ensure that more patients benefit from this cancer treatment.”
Eribulin Mesylate Injection is a cancer medication that disrupts the growth of cancer cells. It was originally approved by the FDA in November 2010 to treat adult patients with locally advanced or metastatic breast cancer whose treatment has not progressed well through other cancer medicines. The FDA expanded its approval in January 2016 to adult patients who have already received anthracycline-containing therapy for advanced or metastatic liposarcoma.
Long Grove Pharmaceuticals received FDA approval for the drug through an Abbreviated New Drug Application (ANDA). The company’s Eribulin Mesylate Injection comes in a single dose vial with a rubber stopper not made with latex. The drug is manufactured in the European Union and is Trade Agreement Act (TAA) compliant.

FLORHAM PARK, N.J — Phathom Pharmaceuticals, Inc. announced the U.S. Food and Drug Administration (FDA) has approved VOQUEZNA® (vonoprazan) 10 mg tablets for the relief of heartburn associated with Non-Erosive Gastroesophageal Reflux Disease (Non-Erosive GERD) in adults. Non-Erosive GERD represents a substantial segment of the U.S. GERD population, affecting millions of individuals suffering from frequent heartburn. This is the third FDA approval for VOQUEZNA, which is also approved to treat all severities of Erosive Esophagitis (EE), also referred to as Erosive GERD, and in combination with antibiotics for the eradication of Helicobacter pylori (H. pylori) infection.
“Today marks a significant milestone for millions of GERD patients as we proudly announce the approval of VOQUEZNA for the treatment of Non-Erosive GERD,” said Terrie Curran, President, and Chief Executive Officer at Phathom. “For decades GERD sufferers had no new class of treatment to turn to in the U.S. This approval provides patients and healthcare providers with immediate access to the first and only FDA-approved treatment of its kind, from a new class of acid suppression therapy, and the power to help provide complete 24-hour heartburn-free days and nights. We are very excited to introduce VOQUEZNA to the broader GERD community and look forward to its potential to help change the way this disease is treated.”
Non-Erosive GERD is the largest category of GERD and is characterized by reflux-related symptoms in the absence of esophageal mucosal erosions. An estimated 45 million U.S. adults living with Non-Erosive GERD, and approximately 15 million are treated with a prescription medicine annually. Despite longstanding treatment options, many patients remain dissatisfied with such therapies and continue to suffer from heartburn symptoms which may impact overall quality of life with episodic heartburn, occurring during the day and at night.
“Millions of patients with Non-Erosive GERD continue to suffer from heartburn despite current treatment options,” said Colin W. Howden, M.D., Professor Emeritus, University of Tennessee College of Medicine. “The pivotal study that led to this approval showed that VOQUEZNA significantly reduced heartburn episodes in patients with Non-Erosive GERD along with an established safety profile. Today’s approval of VOQUEZNA provides physicians with a novel, first-in-class treatment that can quickly and significantly reduce heartburn for many adult patients.”
This approval is supported by the positive results from the PHALCON-NERD-301 study (NCT05195528), a Phase 3 randomized, placebo-controlled, double-blind, multi-site U.S. study evaluating the efficacy and safety of VOQUEZNA for the daily treatment of adults with Non-Erosive GERD. The trial enrolled 772 adult patients with Non-Erosive GERD who experienced four or more days of heartburn per week, with the majority having six to seven days of heartburn per week, and compared patients treated with VOQUEZNA 10 mg to placebo in the relief of heartburn over four weeks. The trial also included a 20-week extension period where all patients received VOQUEZNA to evaluate long-term treatment.
In the trial, VOQUEZNA quickly and significantly reduced heartburn with daily treatment through week 4. VOQUEZNA demonstrated the power of more complete all-day and all-night heartburn-free days with significantly more 24-hour heartburn-free days through week 4 versus placebo, the primary endpoint. The mean percentage of heartburn-free days for patients taking VOQUEZNA was 45% versus 28% for placebo (p<0.001), and the median percentage of 24-hour heartburn-free days was 48% versus 17%, respectively. Improvements for those taking VOQUEZNA were also seen in the percentage of each of heartburn-free days and nights, in addition to the percentage of days without rescue antacid use. Results from the pivotal study were previously presented at Digestive Disease Week® (DDW) 2024 and also published in Clinical Gastroenterology and Hepatology.
The most common adverse reactions (≥2%) reported in patients treated with VOQUEZNA during the four-week placebo-controlled trial include abdominal pain, constipation, diarrhea, nausea, and urinary tract infection. Upper respiratory tract infection and sinusitis were also reported in patients who received VOQUEZNA in the 20-week extension phase of the trial.

MINNEAPOLIS, MN – Certain drugs used to treat urinary symptoms due to an enlarged prostate may be associated with a reduced risk of dementia with Lewy bodies, according to a study published in the June 19, 2024, online issue of Neurology®, the medical journal of the American Academy of Neurology. Dementia with Lewy bodies is a progressive neurodegenerative disorder that can cause memory and thinking issues, movement problems and issues such as hallucinations.
The results do not prove that these drugs reduce the risk of dementia with Lewy bodies; they only show an association.
“These results are exciting because right now there are no drugs to prevent or treat dementia with Lewy bodies, which is the second most common neurodegenerative type of dementia after Alzheimer’s disease,” said study author Jacob E. Simmering, PhD, of the University of Iowa in Iowa City. “If we can determine that an existing drug can offer protection against this debilitating disease, that has the potential to greatly reduce its effects.”
The study looked at male participants taking different types of drugs to treat urinary problems caused by an enlarged prostate, a common problem for older men. The drugs terazosin, doxazosin and alfuzosin could block brain cell death by activating an enzyme important for energy production in brain cells. Previous studies have shown an association between these drugs and Parkinson’s disease, which is similar to dementia with Lewy bodies.
For the study, researchers looked at a health information database for male participants who had started taking one of those three drugs. They were compared to people who took two other types of prostate drugs that do not activate the same enzyme—tamsulosin and the 5a-reductase inhibitors finasteride and dutasteride, called 5ARIs.
Overall, there were 126,313 people taking terazosin, doxazosin or alfuzosin, 437,045 people taking tamsulosin and 80,158 people taking a 5ARI. Researchers followed the participants for an average of three years to see who developed dementia with Lewy bodies.
There were 195 people who developed the disease among those taking terazosin, doxazosin or alfuzosin, for a rate of 5.21 cases per 10,000 people per year. Among those taking tamsulosin, there were 1,286 cases, for a rate of 10.76 per 10,000 people per year. Among those taking 5ARIs, there were 193 cases, for a rate of 7.78 per 10,000 people per year.
Once researchers matched the groups by age, other health conditions and other factors that could explain the differences between groups, they found that people taking terazosin, doxazosin or alfuzosin were 40% less likely to develop dementia with Lewy bodies than people taking tamsulosin and 37% less likely than people taking the 5ARIs. The risk of developing the disease was similar among those taking tamsulosin and the 5ARIs.
“More research is needed to follow people over time and determine whether there is a cause-and-effect relationship here, but it is promising to think that these drugs could have a protective effect on this disease that will likely affect a larger number of people as the population ages,” Simmering said.
Since only male participants were included in the study, the results may not apply to female participants. Another limitation of the study is that dementia with Lewy bodies can be difficult to diagnose, so it’s possible that not all people with dementia with Lewy bodies were correctly diagnosed.

MINNEAPOLIS, MN – For people with relapsing-remitting multiple sclerosis (MS), a new study has found that the drug ofatumumab is more effective than teriflunomide at helping people across racial and ethnic groups reach a period of no disease activity. The study is published in the July 17, 2024, online issue of Neurology®, the medical journal of the American Academy of Neurology. Ofatumumab, a monoclonal antibody, is a newer drug for treating MS. Teriflunomide, an immunomodulatory agent, has been available for over a decade.
MS is a disease in which the body’s immune system attacks myelin, the fatty white substance that insulates and protects the nerves. Symptoms may include fatigue, numbness, tingling or difficulty walking. Relapsing-remitting MS is the most common stage of the disease, marked by symptom flare-ups followed by periods of remission.
“Ethnically diverse groups, including Black and African American, Hispanic and Latino, and Asian individuals, are consistently underrepresented in clinical trials, limiting the data available to help make the best treatment decisions for people in these groups,” said study author Mitzi Joi Williams, MD, of Joi Life Wellness MS Center in Atlanta and a Fellow of the American Academy of Neurology. “Our study examined the efficacy and safety of ofatumumab in diverse populations. We found overall the drug was effective and safe across racial and ethnic groups.”
The study was a post hoc analysis of two previous studies, meaning the researchers looked back at data already collected to more closely examine racial and ethnic differences.
The study involved 1,882 participants, of which 3% self-identified as non-Hispanic Black, 4% as non-Hispanic Asian, 8% as Hispanic/Latino and 82% as non-Hispanic white. The remaining participants were classified as “other/unknown.”
One half of participants received 20 milligrams (mg) ofatumumab every four weeks. The other half received 14 mg of teriflunomide once daily. Participants were followed for two years.
Researchers examined disease activity. No disease activity meant participants had no new relapses with symptom flare-ups, no change in disability and no new lesions in the brain or spine detected with an MRI scan.
Over the study, 33% of non-Hispanic Black participants taking ofatumumab had no disease activity compared to 3% taking teriflunomide. Among non-Hispanic Asian participants, the percentages were 43% and 22% respectively. For Hispanic/Latino participants, 37% and 19%, and for non-Hispanic white participants, 37% and 17%. The proportion of people treated with ofatumumab who had no disease activity was consistent among all race and ethnicity groups.
Rates of experiencing side effects were similar for all groups.
“Determining whether there are differences in how people respond to MS therapies is of great importance so that ultimately, each person is given the most effective treatment for them,” said Williams. “Underrepresentation of diverse populations continues to be an issue in research. Future studies should strive to enroll racially and ethnically diverse groups to better inform treatment decisions.”
The study was supported by Novartis Pharmaceuticals Corporation, the maker of ofatumumab. A limitation was that the original studies examined in this analysis were not designed to examine the efficacy and safety of the drugs based on race and ethnicity.

BOSTON, MA — A new partnership between Boston-based Clearway Health, a company partnering with hospitals and health systems to build and strengthen specialty pharmacy programs and Baptist Health, a full-spectrum health system with nine acute care hospitals headquartered in Louisville, Kentucky, was formalized to improve access to payor networks. Entryway into payor networks will aim to improve availability of prescription medications at more affordable prices.
Baptist Health opened a new centralized pharmacy for its healthcare system in June. The partnership with Clearway Health will break down barriers to allow the entire health system, which has 11 existing retail pharmacies across the system, as well as the new central fill pharmacy to unlock opportunities often inaccessible to local or regional hospitals, including access to medications with payor lockouts.
The improved pathway to these medications at more affordable prices will help to reduce care fragmentation by allowing the clinical team to manage the care of more of their patients across the continuum, including their medications and supplies. The health system's improved financial margin will help provide additional and much needed healthcare services to patients and the local community.
"Baptist Health is transforming specialty pharmacy services --not only for our health system, but for hospitals across the country in setting a new industry standard," said Nilesh Desai, MBA, BS, RPh, CPPS, chief pharmacy officer at Baptist Health. "Having an expert partner like Clearway Health to navigate challenging payor networks is a tremendous advantage for our program's growth. In just one year, this work will generate nearly $100M in incremental revenue that will allow Baptist Health to continue to provide essential healthcare services for the communities it serves."
To help hospitals and health systems gain access to life-saving medications for their patients and keep patient care integrated, optimizing relationships with payors is crucial to the success of a specialty pharmacy program and helps to lower costs for all parties involved including the patients, health system and payors.
"Clearway Health supports health systems at every point of their pharmacy and specialty pharmacy journey," said Allison Arant, senior vice president, client development and marketing, Clearway Health. "We're honored to serve as Baptist Health's partner as they launch the fast-tracked expansion of their program. In the first 30 days of our partnership, we unlocked access to the first payor and look forward to continued growth and success together."

MINNEAPOLIS and ST. PAUL, MN — Myogenica, a University of Minnesota startup company, announced U.S. Food and Drug Administration approval for an Investigational New Drug application for MyoPAXon — an induced pluripotent stem cell-derived muscle stem cell product to regenerate skeletal muscle. A pending clinical trial would evaluate the safety, tolerability and engraftment of MyoPAXon in patients with Duchenne muscular dystrophy (DMD).
Dr. Peter Kang, a pediatric neuromuscular neurologist and director of the Greg Marzolf Jr. Muscular Dystrophy Center at the University of Minnesota Medical School, would lead the proposed early-stage clinical trial. Kang and the clinical research team plan to administer intra-muscular injections of MyoPAXon in non-ambulatory adult DMD patients and monitor any potential site reactions or immune response and assess for the presence of dystrophin-producing myofibers.
"We believe stem cells have enormous potential as a tool for muscle regeneration in muscular dystrophy and the timing is perfect to move toward a human clinical trial of this type of therapy in Duchenne muscular dystrophy," said Kang.
If the proposed trial provides positive outcomes, the team will plan on initiating a mid-stage study targeting other muscles and evaluating muscle function. Because MyoPAXon is not specific for any genetic mutation, it has potential use as a treatment for a range of other muscular dystrophies, as well as other muscle degenerative conditions.
"After many years of basic and preclinical work, we are thrilled to finally have the FDA approve an IND application for an iPSC-derived myogenic cell product. This has been a tour de force and we are excited with what the future holds," said Perlingeiro.

A recent multi-institutional study has uncovered troubling trends in opioid prescriptions for young patients undergoing surgery, with 1 in 6 youths filling an opioid prescription prior to their procedure. Even more concerning, 3% of these patients continue to fill opioid prescriptions three to six months after surgery, indicating potential opioid dependence. The study, which includes researchers from Children’s Hospital of Philadelphia (CHOP), Massachusetts General Hospital, University of Pennsylvania Perelman School of Medicine, and Stanford Medicine, highlights the urgent need for better guidelines to prevent unnecessary opioid prescriptions and to identify patients at risk for persistent use. The findings were published in the journal JAMA Network Open.
Each year, approximately 1.4 million youths undergo surgery in the United States. These patients are particularly vulnerable to opioid-related harms. Despite efforts to reduce opioid prescriptions, clinicians must be vigilant about the risk of addiction in adolescent patients, who may be susceptible due to genetic, neurobiological, and social factors. Previously, there was limited knowledge about the risks of persistent opioid use among adolescents and the timing of initial and refill prescriptions.
"While prior analyses have shown a decline in opioid prescriptions in general, following surgical opioid prescribing recommendations remains a critical issue, especially for adolescents who are more inclined to engage in risk-taking behavior," said Dr. Tori N. Sutherland, the study’s first author and an attending anesthesiologist at CHOP. "Our study found that these patients are still filling prescriptions that are either not recommended or are in excess of what they may need. They are also filling prescriptions up to two weeks before surgeries not associated with severe pre-operative pain, putting young patients at risk for developing persistent use throughout their lives as they transition into adulthood."
The study analyzed data from a national insurance database of privately insured patients aged 11 to 20 who underwent 22 different surgical procedures, either common or associated with severe postoperative pain requiring opioids. None of these patients had taken opioids prior to their surgeries.
Out of over 100,000 patients, 46,951 (46.9%) filled an opioid prescription, with 7,587 (16.2%) of these prescriptions filled up to two weeks prior to surgery for procedures unlikely to cause severe preoperative pain. Furthermore, 6,467 (13.8%) patients filled a second opioid prescription, and 1,216 (3.0%) continued to fill prescriptions between 91- and 180-days post-surgery.
One key finding was that severe pain following surgery was not linked to persistent opioid use. Instead, patients with pre-existing chronic pain, who typically underwent procedures associated with mild or moderate pain manageable with non-opioid medications, were more likely to develop persistent opioid use.
"We believe this study underscores the need for establishing a standard of care for patients who undergo these procedures," said Dr. Scott Hadland, the study’s senior author and Chief of Adolescent and Young Adult Medicine at Mass General for Children and Associate Professor of Pediatrics at Harvard Medical School. "Effective pain management is critical and sometimes requires opioids, but clinicians also need to ensure they are not further contributing to the opioid addiction crisis, particularly with young patients."
Source: Children’s Hospital of Philadelphia (CHOP), news release, July 11, 2024

ROSEMONT, IL — Long Grove Pharmaceuticals announced today it received FDA approval of Premix Vasopressin in its most commonly used concentrations.
The company will offer the following concentrations in early Fall 2024:
- 20 units/100 mL (0.2 units/mL) in 0.9% sodium chloride
- 40 units/100 mL (0.4 units/mL) in 0.9% sodium chloride
“We’re focusing on the areas of greatest need in critical care, and the FDA approval of Premix Vasopressin demonstrates this commitment. Our extensive hospital pharmacy and pharmaceutical industry experience enables us to develop differentiated pharmaceuticals designed to specifically meet our customers’ and patients’ greatest areas of need,” said Peter Karas, Chief Commercial Officer at Long Grove Pharmaceuticals.
Vasopressin in Sodium Chloride Injection is generally used to increase blood pressure when other measures have failed for patients in critical hypotensive shock. Hospital pharmacies throughout the U.S. have a critical need for premix vasopressin with a long shelf life. Long Grove’s new offering will provide immediate value to hospital pharmacies and their patients.
Long Grove Pharmaceuticals introduced its first product to customers in 2022. The company is improving the generic supply chain by developing complex formulations, addressing manufacturing challenges, and achieving regulatory approvals in difficult environments.
“We believe that collaborative and reliable partnerships with manufacturers, developers, suppliers, and customers are essential for sustaining a healthy drug supply chain,” explained Mr. Karas.